Tool helps evaluate students’ palliative care skills
Instrument developed to test end-of-life treatment readiness
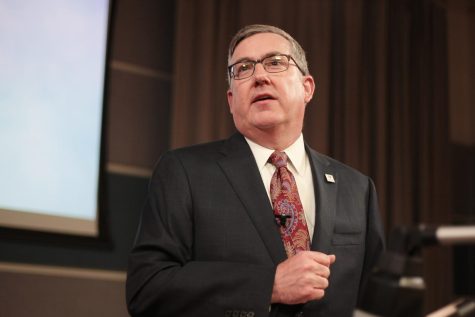
WSU Vancouver professor Andra Davis says palliative care is the practice of providing support to patients who have been diagnosed with a life-limiting illness.
November 14, 2018
An assistant professor from WSU Vancouver and an assistant professor from University of Alabama received an award at the National League for Nursing Educational Summit in September for a tool they developed to help measure nursing students’ competency for end-of-life care.
Andra Davis, an assistant professor at WSU Vancouver, and Megan Lippe, an assistant professor at Alabama, worked together to write the grant which consists of two phases, Davis said.
The first phase is a literature review which sets the standards of what the core elements of palliative care are, according to the abstract for the National League of Nursing grant. The second phase includes taking their model to focus groups and administering surveys to experts in the nursing field to evaluate the tool and provide feedback.
Palliative care is an interdisciplinary practice of providing support to patients who have been diagnosed with a life-limiting illness, Davis said.
“It takes a village of providers that come together to provide and support patients and families,” she said.
The Dorothy Otto Research Award gave them a $25,000 grant for their measure.
“It really was quite an honor to get that grant,” Davis said. “They’re really prestigious and hard to get.”
In January 2017, the End-of-Life Nursing Education Consortium, or ELNEC, took its previous curriculum designed for practicing nurses and made it geared toward students, Davis said. Prior to this there was nothing for undergraduate students to teach the basic skills of providing end-of-life care.
“We need to start having those conversations before people are on the doorsteps of death and you have to really evaluate what they want in their life,” she said.
Davis worked as an oncology nurse and provided palliative care to patients before teaching. She said many students expressed fear over having difficult conversations with patients who have life-limiting illnesses. Students would not want to enter the room and there was a lot of “angst” around it, she said.
“This is really something that mattered a whole lot,” Davis said. “I felt like nurses need to be able to not be afraid of this.”
The idea for the measure stemmed from there not being any written literature about how to tell if students were competent in the core skills of end-of-life care. Davis reached out to the ELNEC about wanting to develop this idea. The tool can be used across the country to evaluate students’ skills in this area, she said.
“It doesn’t matter where they’re going to work, they’re going to deal with people who have life-limiting conditions,” she said.
Only 200 schools have picked up the ELNEC curriculum and are using it with their students. Although there is already so much being packed into the curriculum, Davis said it is a fundamental aspect of care for students and must be taught.
“I felt that it was an honor to be with people, meet them where they’re at and help them move through this difficult time,” she said. “I wanted to be part of that.”