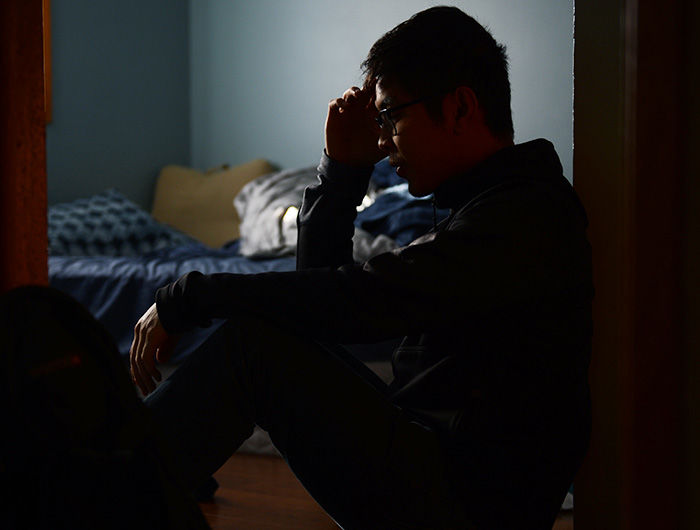
Making mental health care more mandatory
People with symptoms of serious mental illness make up 4 percent of the population, yet account for 30 percent of the chronically homeless.
October 25, 2016
The treatment and maintenance of mental health is the new battle against polio.
As a society, we’ve finally come to seriously address the presence of mental illness and establish resources for treating it.
We’ve greatly diminished the mystique around the subject, but now we need to seriously consider making treatment for mental health less voluntary.
In the not-too-distant past, inoculations against childhood diseases were mandatory, at least for children to be allowed in schools.
The same should be increasingly true for mental illness – in the same way we vaccinate for the good of our learning communities, we should be searching for ways to sensitively require treatment through more robust intervention.
I am not talking about mass institutionalization for health issues like chronic depression or anxiety. However, after a certain point, the issue becomes more detrimental for a community like WSU to not intervene on behalf of a person’s well-being.
Though still highly controversial, the trend of advocating for humane forms of involuntary treatment, especially for more serious mental illnesses, continues to gain traction.
Haley Sweetland Edwards of Time Magazine wrote on Feb. 20, 2015, that court-ordered Assistant Outpatient Treatment (AOT) programs are finding favor even in liberal strongholds.
“In many parts of the country, including liberal bastions such as the San Francisco Bay Area, lawmakers are beginning to embrace AOT programs on both fiscal and humanitarian grounds,” Sweetland Edwards wrote. “Although people with symptoms of serious mental illness make up only about 4 percent of the U.S. population, they account for 15 percent of state prisoners, 24 percent of jail inmates and as much as 30 percent of the chronically homeless population.”
WSU should also consider embracing stronger intervention policies.
Those in our community who suffer from mental health concerns but consistently refuse treatment should at some point have certain holds placed upon their continued academic advancement unless they receive treatment.
The university fundamentally disservices a student by keeping them enrolled when they will be incapable of academically succeeding due to a mental or physical condition requiring treatment.
I say all of this as a person with my own mental health concerns. I suffered from an eating disorder my sophomore year of undergraduate education.
However, I readily sought treatment, especially after my parents threatened to remove me from school if I did not receive treatment.
In hindsight, my best interests were served when I no longer had a viable choice except to get help.
David Marcus, professor and chairman of the WSU psychology department, wrote in an email that this tradeoff between individual autonomy and addressing concerns of well-being is precisely the reason why this subject seems so controversial.
“Involuntary commitment is complicated because someone cannot be deprived of their civil rights unless they are an imminent danger to themselves or others,” Marcus wrote. “It is difficult to know what to do about people who would benefit from treatment but who refuse the treatment.”
Lloyd I. Sederer in an Oct. 8, 2013, column for Psychology Today described how involuntary psychiatric hospitalization ended poorly for three of his patients, but that does not mean he believes patient-centered care should not require intervention.
He describes how this care should avoid the traumatic experience of police arrival, being tied to a gurney and forced into a hospital stay.
“This requires giving people with mental illness, their families and communities, and our mental health system the means to identify problems early, typically in adolescence, and new methods of engaging people with illness in effective treatments that also support their families,” Sederer wrote.
Likewise, the university should assertively intervene if it truly values creating a healthy learning environment for all students.
Reports through WSU’s AWARE Network, a resource that allows individuals to report on the physical and psychological well-being of other students, are not enough.
At some point, it should be considered in the better interests of a student that treatment be required for continued enrollment.
By keeping mental health treatment completely voluntary, we dispense with collective responsibility for each other.
For example, if someone’s roommate engages in self-harm but does nothing to help them, it sends a poor message about our willingness as Cougs to care for our fellow Cougs.
A policy of any form of assertive mental health intervention should be premised on this notion of collective responsibility, a notion of true care for our fellow human being.
Simply reporting incidences after the fact, creating profiles and offering resources is not enough.
Editor’s note: This column is part of a head-to-head series. Read the other side here.
Tyler Laferriere is a graduate student pursuing his master’s in economics from Phoenix, Arizona. He can be contacted at 335-2290 or by [email protected]. The opinions expressed in this column are not necessarily those of the staff of The Daily Evergreen or those of The Office of Student Media.