‘Cancer therapy is a heartbreaker’
WSU researchers identify FOXO1 as protein associated with heart damage, cancer drugs
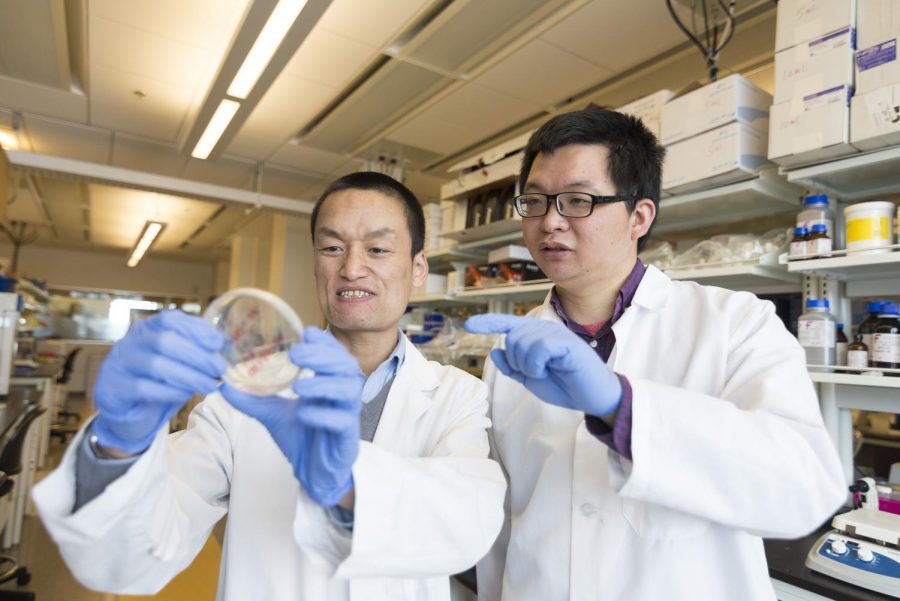
Zhaokang Cheng works with postdoctoral research associate Peng Xia in their lab. Cheng said heart disease is one of the main causes of death in cancer survivors, other than cancer recurrence.
April 24, 2020
Researchers in the College of Pharmacy and Pharmaceutical Sciences at WSU Spokane recently pinpointed a protein that plays a critical role in heart damage caused by chemotherapy drugs.
Zhaokang Cheng, assistant professor and senior author on the study, said cancer treatments have improved a lot in the past several decades and there are more cancer survivors now than ever. However, certain treatments often lead to heart disease. Other than cancer recurrence, heart disease is a leading cause of death in cancer patients.
Though chemotherapy drugs kill cancer cells, they also cause side effects. Cheng’s research examined how these drugs, specifically a class of chemotherapy drugs called anthracyclines, can be toxic and could cause heart damage.
Doxorubicin, a specific type of anthracycline, is used to treat leukemia, lymphoma, breast cancer and many other cancers, Cheng said.
A previous study from the University of North Carolina at Chapel Hill found that patients who are treated with doxorubicin may have their heart sizes decrease. Cheng said this can be caused by a decrease in cell size (atrophy) or a decrease in the number of heart cells.
If there is a decrease in cell number, that means there is an increase in cell deaths, or apoptosis, Cheng said. Heart cells cannot proliferate, meaning they cannot regenerate quickly after many die.
Cheng and other researchers tested doxorubicin in mice in order to determine what causes a decrease in heart size when exposed to the drug.
In a previous paper published in 2018, Cheng’s team studied how a protein called CDK2 is involved in a signaling mechanism for cell death. A signaling mechanism is a molecular pathway involving multiple molecules or proteins which signal a cell to do something.
In their current research, they pinpointed FOXO1, another protein involved in the signaling mechanism, Cheng said.
When CDK2 is activated by doxorubicin, it activates the FOXO1 protein. FOXO1 is then involved in regulating a gene called Bim. When Bim is expressed, cell death occurs. FOXO1 is also involved in regulating a gene called MuRF1, which when activated, leads to atrophy.
Cheng said children are generally more sensitive to chemotherapy, which might mean this signaling pathway is less active in adults. Children may be more likely to experience decreased heart size because of this.
Once doxorubicin has been used on a patient, side effects can occur up to 10 or 20 years after treatment. This is called chronic toxicity, Cheng said.
In future studies, he said they would like to research how to prevent both acute (short-term) and chronic (long-term) toxicity caused by chemotherapy.
Cheng’s team hypothesized that inhibiting or blocking FOXO1 would prevent cell death. When they tested this, they found that hearts treated with a FOXO1 inhibitor and doxorubicin stayed the same size and maintained function.
Cheng said they hope to test this finding in clinical trials. Pairing doxorubicin with a FOXO1 inhibitor could lead to effective cancer treatment without heart damage.
“Chemotherapy, cancer treatment, can break the heart … it’s a heartbreaker,” Cheng said. “We’re trying to stop it from doing that; trying to repair a broken heart.”
Students who are interested in future research may contact Cheng by email at [email protected] or apply online for research positions.