Pullman Regional Hospital awarded $450,000 for residency program
Hospital close to reaching $1.55 million goal; construction for the program may begin in the fall
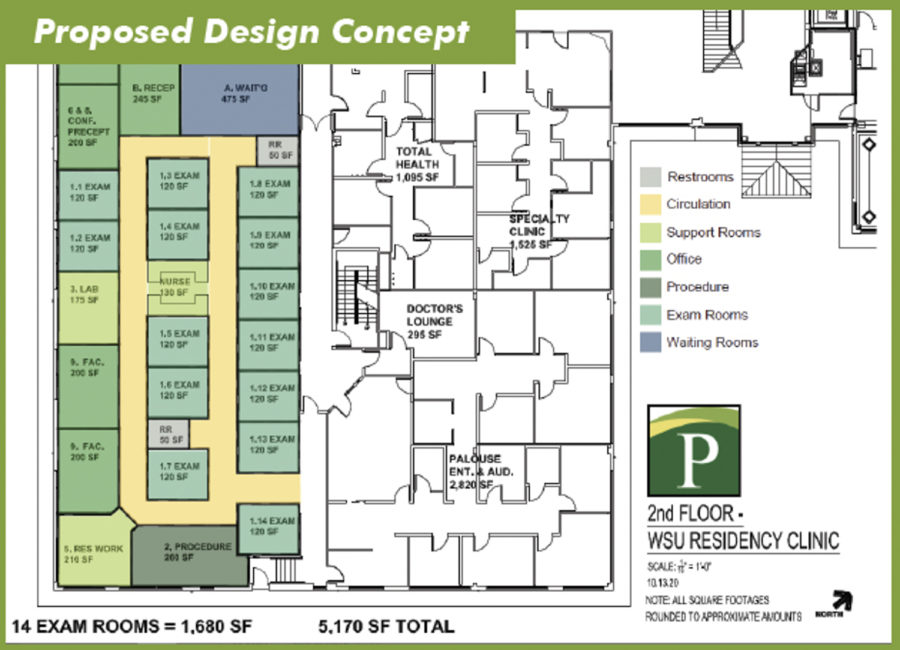
COURTESY OF PULLMAN REGIONAL HOSPITAL
The residency program will take over PRH’s administrative offices. About 5,000 square feet will be used to create 14 exam rooms, a waiting area, study area and faculty offices.
April 22, 2021
The M.J. Murdock Charitable Trust recently awarded Pullman Regional Hospital $450,000 for the clinical and education space for the proposed WSU Family Medicine Residency Program.
Last year, PRH submitted a letter of inquiry to the foundation and submitted a proposal for a grant in the fall, said Rueben Mayes, PRH Foundation chief development and external relations officer.
The hospital was notified in October that the proposal had been accepted. Representatives from the foundation visited the site for the residency program in December, he said
Mayes said the application itself included what PRH intended to do with the money, the cost of the residency program and what impact the grant would have on the project.
Representatives reviewed information from the application and site visit before awarding the grant, he said.
Creating the residency program aligns with the WSU Elson S. Floyd College of Medicine’s mission of focusing on rural and underserved communities, said Christina VerHeul, College of Medicine director of communications, marketing and strategic operations.
The College of Medicine was created in 2015 with the goal of having more students from rural communities in Washington pursue a medical career, she said.
VerHeul said the College of Medicine applied around November for accreditation by the Accreditation Council for Graduate Medical Education. The College of Medicine will be informed about whether or not they are accredited by the summer.
“Assuming we receive that accreditation, we can then actually move forward with truly starting the residency and recruiting applicants to the residency,” she said.
PRH is close to reaching its $1.55 million goal for the renovations to accommodate the residency program, said Alison Weigley, PRH director of external relations.
Mayes said the residency program will take over PRH’s administrative offices, which will move to a different location offsite.
About 5,000 square feet will be used to create 14 exam rooms, a waiting area, study area and faculty offices for the program, Weigley said.
She said construction for the residency program should begin in the fall. The goal is to welcome physician residents in June 2022.
Dr. Stephen Hall, family medicine physician at Palouse Medical, is the developing program director. He has worked at Palouse Medical for more than 30 years and had a long-term vision for a residency program in Pullman, Weigley said.
PRH will accept three people for the first year of the residency program and three more every year after that, she said.
However, the cap for residents is nine because it ensures residents receive the best education and experience possible given the relatively small size of the hospital, VerHeul said.
VerHeul said it can be challenging to create these types of programs because of the small number of resources.
Weigley said creating the residency program is a good solution to reducing the shortage of family medicine physicians nationwide and in Eastern Washington.
“Residency programs are a really great pipeline to recruiting and retaining physicians,” she said.
Research shows some residents will stay in the region where they completed their three years of residency because that is where they trained how to be a doctor, Mayes said.
Mayes said someone that receives an undergraduate degree, then their medical degree, and then does a residency in the same location has a 70 percent chance of staying within 100 miles to practice medicine.
There are various reasons why there is a shortage of physicians in rural communities. The salaries for physicians in rural areas are often smaller than salaries in larger communities, VerHeul said.
Students often graduate medical school with debt, so it is not always financially viable for medical students to practice medicine in a rural community, she said.
Mayes said the ability to have enough primary care physicians in a growing community is critical.
“We’re just really grateful that we were selected [for the grant] and that they are excited to be part of an organization that’s trying to solve a big problem in Eastern Washington,” he said.