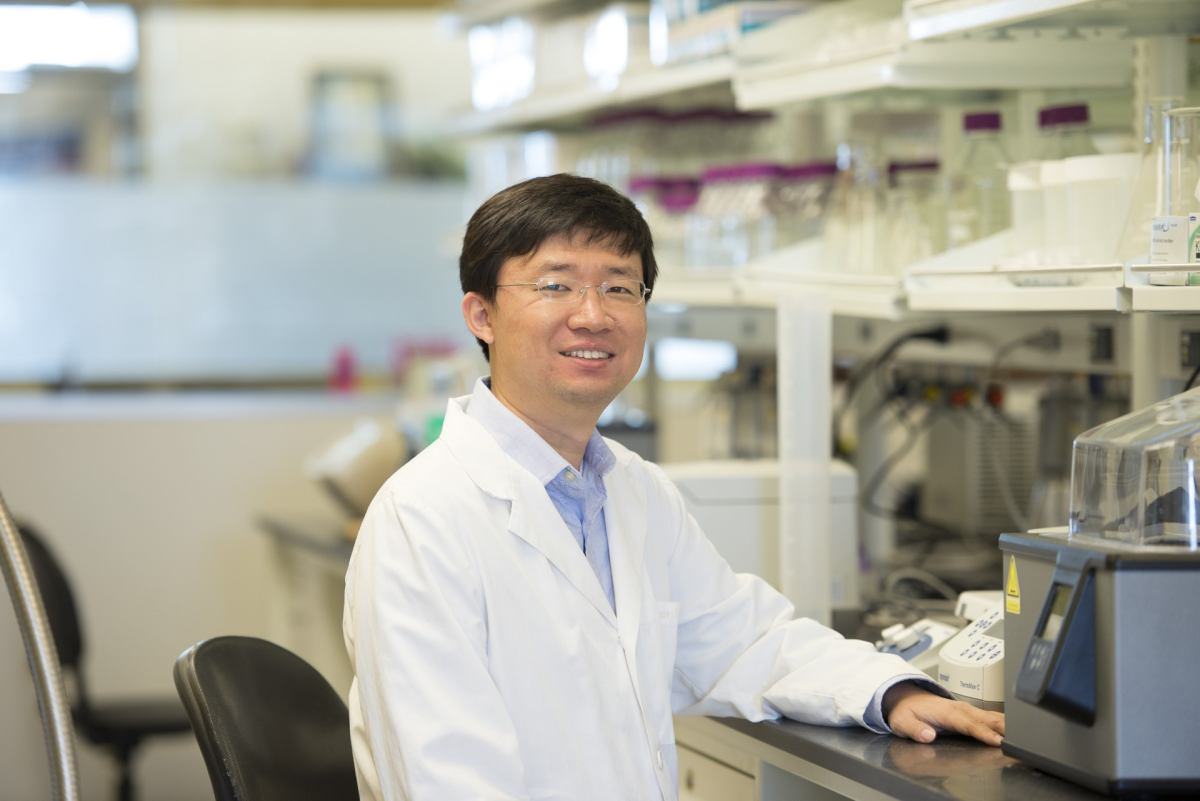
Innovations in prostate cancer treatment have recently been made by scientists including Dr. Jason Wu, WSU Pharmaceutical Sciences Associate Professor, and Dr. Tyler Bland, UI Clinical Assistant Professor and former WSU postdoctoral researcher.
Their project began in 2017 when those in Wu’s lab began a project to understand how prostate cancer is linked to neuronal signaling or the communication between cells, Bland said. One particular method of cell interaction that interested them was acetylcholine, which is released by neurons to the muscles in order for them to move and fire.
“One of the main drivers of prostate cancer is the androgen receptor. The male sex hormones, androgens, prostate cancer usually feeds off of that. The sex hormones bind to the receptor [and] that causes it to grow,” he said. “I was wondering if there was some sort of interplay between the neurons releasing acetylcholine and that enhancing antigen receptor signaling to promote it.”
Unfortunately, this did not have any results, Bland said. Later on, however, they thought to introduce docetaxel into the study.
“We had chemotherapeutic docetaxel, which is a common chemotherapeutic usually used in late stage prostate cancer, and I thought, what if I mix these two together? What if I take a drug that blocks acetylcholine’s ability to signal and combine it with the chemotherapeutic,” he said. “It turned out, when I combined them, the cells died even better.”
These findings that acetylcholine increases the ability for chemotherapeutics to kill cancer cells led them to study muscarinic receptors and a protein known as CHRM, Bland said.
They then introduced drugs that served to block these receptors, one drug for an overactive bladder and another for irritable bowel syndrome, with the latter being the one used for the study, Bland said. Drugs for irritable bowel syndrome contain dicyclomine, an inhibitor of CHRM1, Wu said.
“We added the irritable bowel syndrome drug and the chemotherapeutic, and it killed the cancer cells a little bit better, just a little bit. And we thought, well, if it’s killing these cancer cells, prostate cancer, typically you start treating with chemo and [it] works for a little bit of time, and then they become resistant,” he said.
Following these findings, they began to investigate if CHRM1 could impact this resistance, Wu said.
“We speculated that maybe targeting this acetylcholine signal pathway through the CHRM1 protein could be used for overcoming the docetaxel resistance in prostate cancer,” he said. “This inhibits the receptor activity of this protein [which can] significantly enhance the docetaxel efficacy in the resistant cells. In other words, [this] can restore the sensitivity of docetaxel in resistant cells.”
The study then began to use chemotherapeutic resistant cells to its cell line which originally contained regular prostate cancer cells, Bland said.
“We got chemotherapeutic resistant cells, and we added the irritable bowel syndrome drug, and nothing happened. Then we added the chemotherapeutic (docetaxel) on, and nothing happened, which made sense because they were resistant. Then we added both, and they all got wiped out,” he said.
With this discovery of the effectiveness of the combination of the drugs, it is hoped that this will serve as an alternative to pre-existing prostate cancer treatment methods, Bland said.
“This is what’s cool, is that you can use this generic drug that’s been around for a long time, [and is] well tolerated because it’s used to treat IBS, whereas most chemotherapeutic agents are pretty nasty,” he said. “We could basically turn the clock back on these resistant cancers. So you use this chemotherapeutic and [the cells] become resistant, [then] you add this other drug on [and] it turns the clock back. Now you can add chemotherapeutic but even less than when you originally started because it’s basically to resensitize them to the chemotherapeutic.”
This makes the treatment more feasible as it does not require FDA approval for a new drug, Wu said.
“I think this is one of the biggest advantages for using dicyclomine,” he said. “We already know the main toxicity profiles and parameters of this drug, so it’s safer to use an FDA-approved drug for our preclinical studies.”
This may also make treatment for late-stage prostate cancer more effective, Wu said.
“When prostate cancer develops into a terminal stage, at that stage, there are very few options available. Docetaxel is one of the very few options,” he said. “[It is] effective but, unfortunately, it will cause, like all drugs, it can cause local resistance usually after six months. So I think our findings may provide a solution.”
The study was funded by the Department of Defense Early Investigator Research Award, which Dr. Bland applied for prior to transferring to UI. The study was able to continue at WSU due to the funds of the grant being transferred to Dr. Tianje Pugh, a postdoctoral researcher from WSU and one of the study’s co-authors, Bland said.
Stock funds from WSU’s College of Pharmacy also served to start and support the project, Wu said. There is also potential for these findings to be applied in research for treating other cancers, including breast and lung cancer.
Dr. Wu and his lab at WSU will carry on with the original prostate cancer research, while Dr. Bland and others at UI will study the potential applications to lung cancer treatment.
Currently, a patent for this discovery has been applied for and is under review. While this study was used on a mouse model with patient-derived prostate cancer tissue as opposed to a full clinical trial with human participants, physicians could use this today, Bland said.
“If we wanted to fully describe and show that this works in humans, we would have to run a clinical trial. The clinical trials are very expensive and [cost] millions of dollars, and we don’t have the funding for that,” he said. “What’s nice is that, because we are taking an existing drug and we’re repurposing it into another area of the clinic, that entry barrier is much much lower.”
Still a clinical trial is needed to test if the combination of drugs is indeed fully safe to use on people, Bland said.
“The [IBS] drug that we’re using, docetaxel, has been used in humans for decades, so we know that’s safe. Do we know that it’s particularly safe when combined with chemotherapy and prostate cancer patients, the answer to that is no,” he said.
Applying these findings to another cancer drug cabazitaxel is also being considered, Wu said.
“It’s also used for treating prostate cancer patients and so we are also trying to test whether dicyclomine [or] any other CHRM1 antagonist can be used to enhance the cabazitaxel’s efficacy,” he said.