Finding an efficient way to treat blindness
Researchers have made prototype aimed at reducing cost of drug delivery to people with eye disease
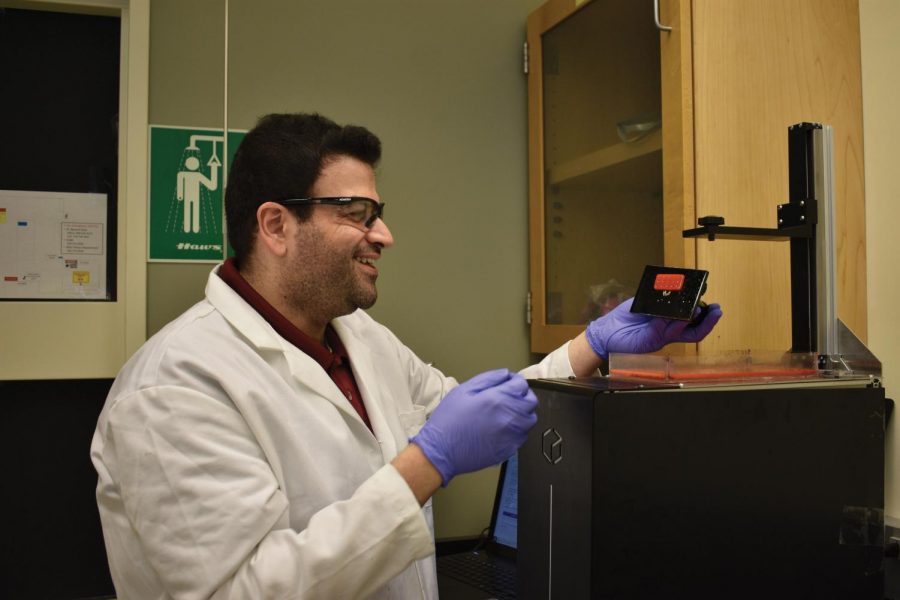
DYLAN GREENE | THE DAILY EVERGREEN
Doctoral student Maher Amer smiles as he finishes 3-D printing a mold for the hydrogel inside the Engineering Teaching and Research Lab building Tuesday. Amer said he was suprised this mold printed. “It’s a process,” he said. “We keep repeating it, but it actually printed.”
June 27, 2018
An assistant professor and a doctorate student at WSU have helped develop a prototype in an effort to make treatment for the two leading causes of blindness in the U.S. less expensive and more effective.
Kuen-Ren Chen is the professor and Maher Amer is the doctorate student. Both are aiming to combat diabetic retinopathy and age-related macular degeneration, the two major eye diseases that damage blood vessels and affect millions of people worldwide.
“These two diseases … once you get it you cannot really cure it,” Chen said. “You can manage it, you can treat it. It’s not reversible.”
Chen and Amer are working on creating a device that would make delivering drugs to the eye to treat these diseases more effective than three common practices used by doctors currently; laser therapy, direct eye injections and eye drop.
The device, called a microneedle array, consists of hundreds of tiny needles put right next to each other to form a cluster.
The prototype for the device they have created is made of plastic, but a $264,000, 18-month exploratory grant from the U.S. Department of Defense will allow them to develop a programmable microneedle array made of hydrogel using a 3-D printer.
The microneedle array will look similar to a contact lens, except it will be much smaller, attach to the side of the eye and be yellow or white instead of transparent.
Amer said the microneedle technology is not new, but the concept of using hydrogel to form a device that easily “locks” and “unlocks” from the eye is unlike anything else.
“No one really puts eye patches in the eye,” he said, “it’s really rare.”
Amer said hydrogel absorbs water, so when it is inserted into the eye it will get bigger and lock itself into place, something current corrective lenses are unable to do.
In order to “unlock” the array from the eye, Amer said a certain density and wavelength of normal light must be shined into the eye to change the chemical structure of the device and make it reject water, causing the array to shrink and detach from the eye.
Current treatments, such as direct eye injections, require patients to go in weekly or monthly to have the drug administrated by their doctor, Chen said.
The microneedle array would allow a patient to put the drug into their eye without having to go to a clinic and it would stay in the eye for roughly four weeks.
“We’re hoping that one day you can basically buy a bunch of contacts and you can do it yourself,” Amer said.
Chen said this would allow the drug to slowly release into the eye with the array over an extended period of time and cause treatment to be more effective and reduce the amount of medication wasted.
Direct eye injections have a high drug concentration when they are first inserted and the concentration significantly decreases over time, requiring patients to receive weekly or monthly injections that can cost nearly $2,000, Chen said.
Chen said the microneedle array eliminates this problem by distributing a constant concentration of the drug while in the eye, reducing the amount of medication that is currently being squandered.
The tiny needles on the array are also less painful than direct eye injections and the most popular treatment that inserts the drug into the eye leaves it there for about two years before being surgically removed, Amer said.
The researchers’ technology would go in the eye and back out without the need for surgery that lacerates the eye and would require stitches to seal it back together.
“Cutting someone’s eye open is not fun,” Amer said. “I don’t want to do it, no one wants to do it.”
Amer said they were already researching microneedles when they found out the DOD was looking for devices that delivered drugs more efficiently, leading them to pursue this project.
“We have the background and the DOD had the problem, the need,” Amer said. “Our background provided the solution.”
Now that the researchers have the funding, Chen said they can turn their prototype into a product they can test. If their concept works, Chen said the device probably won’t be made available to patients for another 10 years.
Despite the long process, Amer said the success of the device would open the potential for it to be used for other things, such as healing bones.
“If the concept is proven it will help a lot of people in so many areas,” Amer said. “It doesn’t have to only be the eye.”