Researchers use math, computers to model spread of COVID-19
Computational epidemiology examines pets, hospitals, border cities
WSU researchers are using computational epidemiology to model the spread of COVID-19.
June 8, 2020
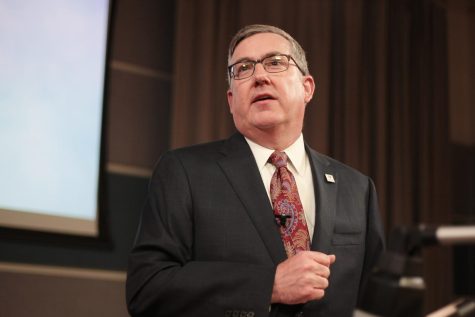
Eric Lofgren and other researchers in his lab at WSU are using computational epidemiology — a combination of computer simulations and complex mathematics — to model the spread of diseases, like COVID-19, in certain populations.
Lofgren, assistant professor in the Paul G. Allen School for Global Animal Health, said he normally works on healthcare-related outbreaks, such as the staph infection MRSA, but has spent most of this year researching the spread of COVID-19.
“We wanted to be able to use our expertise to help and look at things that are societally important and impactful to the field,” he said.
Lofgren researches the spread of diseases in very structured settings, such as hospitals, schools and jails. These are places where people have a specific way or pattern of interacting with others, he said.
Changing certain activities, like canceling recess or lunch for all classes at elementary schools, could minimize the spread of disease, he said.
Lofgren receives some funding from the Centers for Disease Control and Prevention. He said he communicates regularly with the CDC so it can incorporate information from his models into briefing documents and recommendations.
Hospitals
Katelin Jackson, graduate research assistant in Lofgren’s lab, said she uses compartment models to examine the spread of COVID-19 in intensive care units. She does this by categorizing individuals as susceptible, exposed, infected or recovered.
Jackson said she also considers social interactions between nurses and doctors, such as meetings to discuss patient care, and what effect changing those interactions could have on the spread of COVID-19.
“The end goal is to look into easy interventions, like limiting social interactions that might not be necessary,” Jackson said. “What we have is people intermingling, and we want to limit that as much as possible without tampering their duties as nurses and doctors.”
A big part of Jackson’s work is staying informed about COVID-19, she said, so she can incorporate new updates into her model.
The model can be applied to intensive care units in many different locations, Jackson said.
Paired communities
Stephanie Sikavitsas Johnson, graduate research assistant in Lofgren’s lab, is examining how the spread of COVID-19 changes when there are different stay-at-home restrictions in paired towns along state borders, such as Pullman and Moscow or Spokane and Coeur d’Alene.
“One of the aspects of the model might be, ‘What happens if one governor shuts everything down and the other doesn’t?’” Sikavitsas Johnson said. “If there’s a delay of one state shutting down, or if they shut everything down at the same time, how does that affect COVID cases on the other side?”
Sikavitsas Johnson said she has to think about ways people interact and places they could be exposed to the virus. This includes going to the grocery store or caring for a sick individual.
People should be careful not to immediately leave once stay-at-home orders are lifted, she said.
“If you’re on the side of the border where the governor says to stay at home, stay there,” Sikavitsas Johnson. “Don’t continue going over to somewhere else because they’re open.”
Household pets
Matthew Mietchen, doctoral candidate in Lofgren’s lab, is attempting to model how household pets and their owners may transmit disease.
“If we find out, say, SARS-CoV-2 does transmit easily between a dog and a human, we want to be able to look at that and say, ‘How does that contribute to the community?’ and, ‘Does it matter?’” Mietchen said. “That’s a big question we ask in math modeling, ‘Does it matter?’”
Mietchen said his research has the potential to change policies about what kind of questions people are asked when they test positive for COVID-19. For instance, instead of being just asked which people they have interacted with, a patient might be asked which people and animals they have interacted with.
Models help researchers perform cost-benefit analyses, Mietchen said. This means they can determine how helpful an intervention would be, and if it is worth implementing to prevent the spread of COVID-19.